 This event held at Warwick University Business School was a full house with over seventy participants active in the area of healthcare modelling – drawing from many areas of the health service, academic research and industry.
This event held at Warwick University Business School was a full house with over seventy participants active in the area of healthcare modelling – drawing from many areas of the health service, academic research and industry.
Keynote Presentations

Dr Geoff Royston is Head of Profession for OR. in the Dept. of Health and works in the Dept’s Strategy Directorate. Work includes developing methods for allocating health care resources to localities, improving communication of clinical risks, reducing waiting times, evaluating NHS modernisation programmes. Recently he has worked on “expert patients” and support for self-care. He was responsible for the concept of “NHS Direct” as a multi-channel service and led the first stages of its implementation. He has directed the programme of DoH work on health applications of digital TV and a satellite TV service “NHS Direct Interactive” which went “on air” in Dec 2004 now reaches 10 million in the UK.
PRESENTATION: Modelling and Simulation in Health – Potential, Achievement and Challenge Geoff Royston Presentation
Commences with some background on recent major developments in UK health care and a short overview on modelling. It provides some illustrations of modelling and simulation in the UK health sector, including some from the work of OR analysts in the DH. The talk then highlights some key issues for the UK health sector in the early 21st century and the challenges and opportunities these present for members of MASHnet.
 Professor Ruth Davies – Head of the Operational Research and Information Systems Group at Warwick Business School. Her expertise is in modelling health systems, using simulation to describe the interaction between the parts in order to evaluate current and potential future policies. Over the past few years she has run several substantial projects, funded by the Department of Health, in order to advise on policy. She has many active roles in this area and was co-editor of the February 2005 Special Issue of the Journal of the OR Society dedicated to “Meeting Health Challenges with OR”.
Professor Ruth Davies – Head of the Operational Research and Information Systems Group at Warwick Business School. Her expertise is in modelling health systems, using simulation to describe the interaction between the parts in order to evaluate current and potential future policies. Over the past few years she has run several substantial projects, funded by the Department of Health, in order to advise on policy. She has many active roles in this area and was co-editor of the February 2005 Special Issue of the Journal of the OR Society dedicated to “Meeting Health Challenges with OR”.
PRESENTATION: OR, Academics and the Health Service Ruth Davies Presentation
Looks at the relationship between OR and the Health Service using a hospital and a disease based case study. Demonstrates that academic research needs to take a broad view, both developing and exploiting new techniques and also taking account of the objectives of a range of stakeholders. Whilst academics are also concerned with implementation and change, they and the “users” will benefit from closer links with practitioners and software developers. We anticipate that MASHnet will facilitate this.
 Dr Mark Elder – CEO of SIMUL8 Corporation, a company he founded in 1994 because a radiology manager could not find simulation software that could answer his simple question: Should I build an additional radiology room, or hire an additional nurse? – Which would best reducing patient waiting times? Since then SIMUL8 Corp as driven forward the idea of simulation as a tool for gathering evidence for change, that works just as well for the service sector as it has for decades in manufacturing.
Dr Mark Elder – CEO of SIMUL8 Corporation, a company he founded in 1994 because a radiology manager could not find simulation software that could answer his simple question: Should I build an additional radiology room, or hire an additional nurse? – Which would best reducing patient waiting times? Since then SIMUL8 Corp as driven forward the idea of simulation as a tool for gathering evidence for change, that works just as well for the service sector as it has for decades in manufacturing.
PRESENTATION: Developing Models of Health Mark Elder Presentation
Mark’s talk uses a number of recent examples of healthcare simulation models to highlight some do’s and don’ts in simulation modelling. He shows us some of the numerical and non-numerical benefits of spending time on modelling.
 Dr Simon Dodds – born and educated in Yorkshire, won an Open Scholarship to read Medicine at Cambridge in 1979. He chose a Part II in Computer Science and after completing his medical degree at St Bart’s Hospital in London he trained in surgery in London, Cambridge and Wessex. At Southampton he was awarded his MS degree in 1994 for research on computer modelling the haemodynamics of occlusive arterial disease and was appointed a consultant vascular surgeon at Good Hope Hospital in 1999. Since then he has combined his experience in medicine, research and computer science to improve vascular surgery services at Good Hope. In 2004 his team were awarded the NHS Innovation Award for Service Delivery for the Leg Ulcer Telemedicine Service. His current projects include the application of discrete event simulation (DES) to the design of improved healthcare processes for which he was awarded the HITEA 2005 Best use of IT in the Health Service for the successful implementation of the DES-designed One Stop Vascular Surgery Clinic.
Dr Simon Dodds – born and educated in Yorkshire, won an Open Scholarship to read Medicine at Cambridge in 1979. He chose a Part II in Computer Science and after completing his medical degree at St Bart’s Hospital in London he trained in surgery in London, Cambridge and Wessex. At Southampton he was awarded his MS degree in 1994 for research on computer modelling the haemodynamics of occlusive arterial disease and was appointed a consultant vascular surgeon at Good Hope Hospital in 1999. Since then he has combined his experience in medicine, research and computer science to improve vascular surgery services at Good Hope. In 2004 his team were awarded the NHS Innovation Award for Service Delivery for the Leg Ulcer Telemedicine Service. His current projects include the application of discrete event simulation (DES) to the design of improved healthcare processes for which he was awarded the HITEA 2005 Best use of IT in the Health Service for the successful implementation of the DES-designed One Stop Vascular Surgery Clinic.
PRESENTATION: Designing win-win-win solutions for improved healthcare performance – it is possible! Simon Dodds Presentation
The current challenges in delivering high quality, cost effective healthcare are not lack of medical knowledge but ineffective delivery of existing knowledge. Applied OR in healthcare delivery has great potential to dramatically improve existing services. Over the last five years these principles were used to redesign the vascular surgery outpatient service at Good Hope Hospital. A discrete event simulation (DES) has been designed that predicted a possible increase of 40% in maximum clinic capacity using existing resources. Simulations were verified by successfully implementing the best model in practice – resulting in a win-win-win outcome for patients, staff and the hospital. The principles and methods of OR/OM require specific knowledge, skills and experience to apply safely. Active diffusion of innovation requires – support for further innovation, appropriate software tools, end-user training, and a programme of training successive waves of early adopters. The goal is the tipping point where the momentum generated is sufficient to complete the paradigm shift to a culture of evidence-based healthcare management.
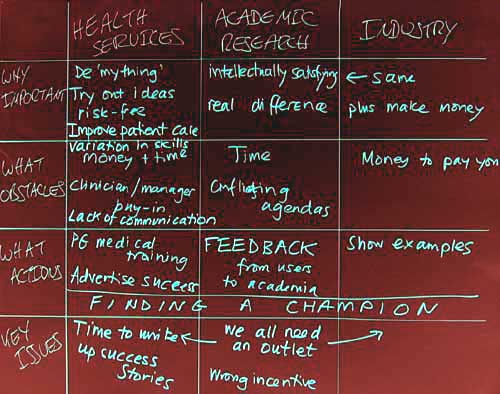
Output From Interactive Sessions
Break-out sessions were held in the afternoon of the launch event in which groups of about eight people were each asked to complete a grid which outlined their responses to a each of the following four questions from the perspective of the three main sectors addressed by MASHnet (i.e. Health Services, Academic Research, and Industry)
- Why is health care modelling and simulation important?
- What are the main obstacles to its successful application?
- What actions can be taken to overcome these obstacles?
- What are the most important issues arising?
Grid Outputs – typed version
Grid from the Pink Group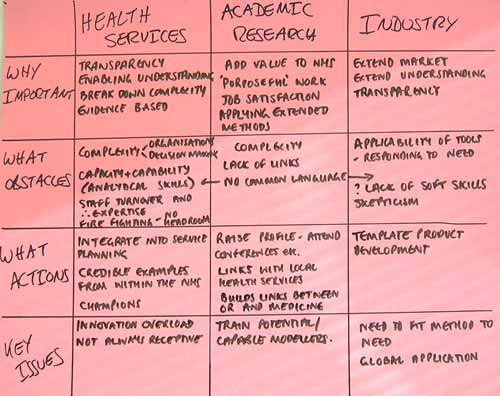
Grid from the Red Group
Grid from the Orange Group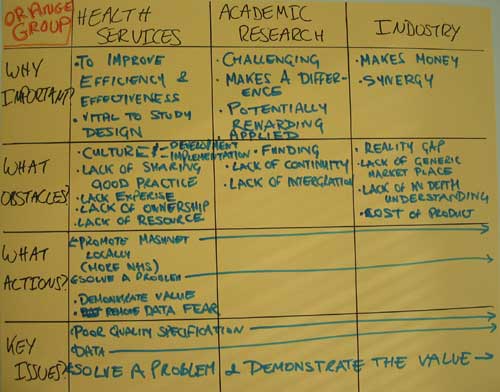
Grid from the Yellow Group
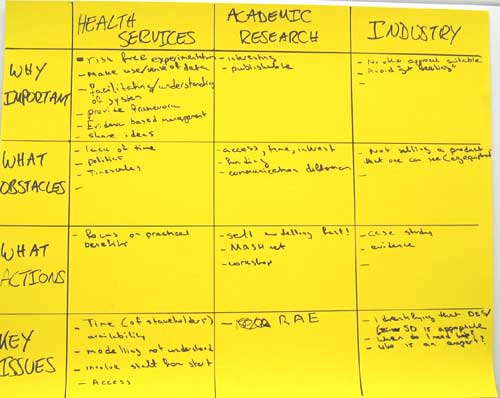
Grid from the Green Group

Grid from the Dark Blue Group
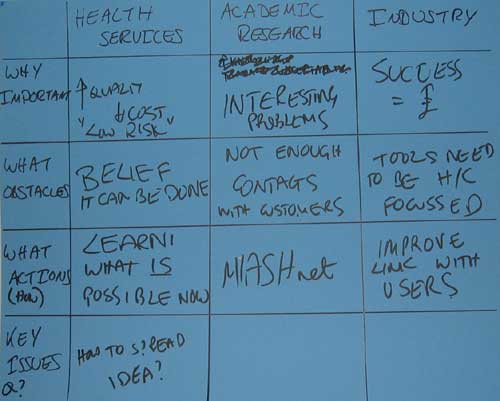
Grid from the Light Blue Group

Grid from the Purple Group

Big Ideas
All participants at the MASHnet launch were asked to fill in a ‘Big Idea’ response form which asked for one idea which would improve the application of modelling and simulation in health care. These responses are listed below:
- Showing success of previous work using modelling to all academics, industry and health
- To look at the application of OR in operational running of health system
- Develop a repository of examples of successful applications
- Develop generic simulation software – joint project for all 3 branches of MASHnet
- You need to work ‘hands-on’ in the operational environment to appreciate actually what happens and who does what, else implementation of anything new is problematic as it will be potentially rejected by staff
- Academics need to ‘buddy-up’ with healthcare practitioners in order to increase awareness and more importantly implementation
- Do not approve any big projects that have not been validated by simulation
- “Go” to the Healthcare community rather than waiting for them to come (workshop, etc.)
- MASHnet representation at NHS conferences e.g. Harrogate and others
- Negotiate central R & D funding champions and National coordination so modelling can be applied across a large number of organisations in a uniform way
- MASHnet to become a more political driver to bring the 3 groups together – target modelling to be centre of health service change
- To look at the beginning – to work together with designers (key designers) to help them to find out the “key” questions in terms of how the healthcare building will operate
- Mashnet and healthcare conferences. Industry and academics working together with a health economy and actually doing some “hands-on” work. Not all healthcare organisations have the appropriate resources – people, time, etc. to be able to apply/use a mode “off the shelf”
- Workshops in regions of NHS
- Plan at least one training event for people to bring real problems and to work with acknowledged practitioner to experience first-hand to see MASH in action
- Every community (health service, academic and industry, etc.) needs to take responsibility for increasing implementation levels
- Developing intra-organisational pathway model
- Facilitating a feedback system so that all modelling work/outcomes get centrally registered
- Need to plan a programme grant application to a research council for a sustained (5-yr) research programme. One element could be a direct comparison of a RCT and DESM head to head
- On-line source of case studies of health service (real applications) projects that have been implemented. Particular emphasis should be on operational level (i.e. hospital). The Modernisation Agency has disseminated some material, e.g. toolkits, but more detailed real examples would be useful
- Find ways to integrate modelling as a key discipline of health-related research alongside the other key disciplines (e.g. statistics, economics, health psychology, etc.)
- Workshops for practitioners, clinicians, and healthcare managers. We need to get the modelling concept across more forcibly
- Hold “problem-drive” days where academics/health care professionals/ industrials meet – healthcare profs. Present current real-life major issues and others brain-storm ways of helping (i.e. put academics on the spot!)
- My mission statement – to de-mystify the building of models to solve real problems
- Publicise to Chief Executives of healthcare organisations in order to raise and support the profile of modelling and encourage ‘buy-in’
- Involve the independent sector of healthcare who might have an easier entry point than existing NHS to show effectiveness of modelling and therefore greater acceptance. Noting that IS is elective not 24×7
- The DoH to promote OR and modelling to NHS executives, managers
- Create a road show of big-hitting OR applications. Show the direct and practical implemental benefits … in 10 mins. Then show this to senior people in NHS
- Have articles about M&S in health service journals. Have presentations about M&S at professional (medic managers) conferences
- Collaborating closely between health care providers and system modelling builders (academics and software developers), clinicians and professionals and also users. Make model simple, valid and also flexible
- Composition of an “Idiots’ Guide” to modelling & simulation aimed at health management and practitioners so that they can get an easier grasp of the benefits
- Promote ‘soft OR’ techniques to highlight problem structuring types of models as well as ‘hard OR’ mathematical models
- Get the appropriate level of abstraction for the representation
- Develop a common language
- Archive of grey literature (much will soon be lost)
- Share modelling successes, particularly with the NHS
- Encourage health service (operations and management) involvement
- Data cleanup and review of ?
- Sharing successful models and learning from each other on a local basis
- Having info on the web: what was done, who did it, how can I contact them
- Whole system modelling that compares like with like to better understand the constraints & complexities of system change
- Find a better name than Mashnet for publicity to NHS; Publicise examples of good modelling and future support
- Incentivise the use of modelling and simulation in planning by sponsoring a Health Service Journal award
- An introduction agency between health service problems and potentially able research/modellers
- A presence at medical conferences/health service conferences and seminars, etc.
- I would like for managers and clinicians to take ownership of the data that is used in modelling and simulation so that they understand its strengths and weaknesses before its use
- To publicise/ inform/advertise/demos of MASHnet activities where NHS people are trained, e.g. to medical students or NHS management courses
- Joint NHS/ University posts in healthcare modelling
- Create a pod of examples where modelling and simulation have worked in health care (how it was implemented, advantages and disadvantages from it). Allow all 3 groups to see what has been done already and what can be applied elsewhere.
- The Government should place tighter controls on budget overspends for Trusts, which would force them to look at more efficient and effective ways of working. This would encourage the use of tools and techniques such as modelling and simulation, as the cause of most overspends is lack of planning
- Chief Executive commitment; Ask smart questions to engage operational staff to access modelling outputs and to implement changes
- Better publication of successful implementations (e.g. Good Hope Hospital)
- Get success stories distributed and create competition for excellence between Trusts
- Long-term strategic goals need to be identified, to develop long-term partnerships between industry, academia and health services – with a view to embedding sectors for knowledge sharing
- Training and skills development for staff who may be required to support their organisation in modelling. Development of standard modelling applications which could be tailored at local level
- Use of modelling & simulation to develop and communicate best practice, both Nationally and Internationally. Library of generic models which can be accessed and used by members
- Working together on (?low-risk) issues to improve each other’s knowledge of opportunities and red herrings
- Work together. Build up standard approaches. Advocate a common software language. Share information and good modelling applications


 This event held at Warwick University Business School was a full house with over seventy participants active in the area of healthcare modelling – drawing from many areas of the health service, academic research and industry.
This event held at Warwick University Business School was a full house with over seventy participants active in the area of healthcare modelling – drawing from many areas of the health service, academic research and industry.
 Professor Ruth Davies – Head of the Operational Research and Information Systems Group at Warwick Business School. Her expertise is in modelling health systems, using simulation to describe the interaction between the parts in order to evaluate current and potential future policies. Over the past few years she has run several substantial projects, funded by the Department of Health, in order to advise on policy. She has many active roles in this area and was co-editor of the February 2005 Special Issue of the Journal of the OR Society dedicated to “Meeting Health Challenges with OR”.
Professor Ruth Davies – Head of the Operational Research and Information Systems Group at Warwick Business School. Her expertise is in modelling health systems, using simulation to describe the interaction between the parts in order to evaluate current and potential future policies. Over the past few years she has run several substantial projects, funded by the Department of Health, in order to advise on policy. She has many active roles in this area and was co-editor of the February 2005 Special Issue of the Journal of the OR Society dedicated to “Meeting Health Challenges with OR”. Dr Mark Elder – CEO of SIMUL8 Corporation, a company he founded in 1994 because a radiology manager could not find simulation software that could answer his simple question: Should I build an additional radiology room, or hire an additional nurse? – Which would best reducing patient waiting times? Since then SIMUL8 Corp as driven forward the idea of simulation as a tool for gathering evidence for change, that works just as well for the service sector as it has for decades in manufacturing.
Dr Mark Elder – CEO of SIMUL8 Corporation, a company he founded in 1994 because a radiology manager could not find simulation software that could answer his simple question: Should I build an additional radiology room, or hire an additional nurse? – Which would best reducing patient waiting times? Since then SIMUL8 Corp as driven forward the idea of simulation as a tool for gathering evidence for change, that works just as well for the service sector as it has for decades in manufacturing. Dr Simon Dodds – born and educated in Yorkshire, won an Open Scholarship to read Medicine at Cambridge in 1979. He chose a Part II in Computer Science and after completing his medical degree at St Bart’s Hospital in London he trained in surgery in London, Cambridge and Wessex. At Southampton he was awarded his MS degree in 1994 for research on computer modelling the haemodynamics of occlusive arterial disease and was appointed a consultant vascular surgeon at Good Hope Hospital in 1999. Since then he has combined his experience in medicine, research and computer science to improve vascular surgery services at Good Hope. In 2004 his team were awarded the NHS Innovation Award for Service Delivery for the Leg Ulcer Telemedicine Service. His current projects include the application of discrete event simulation (DES) to the design of improved healthcare processes for which he was awarded the HITEA 2005 Best use of IT in the Health Service for the successful implementation of the DES-designed One Stop Vascular Surgery Clinic.
Dr Simon Dodds – born and educated in Yorkshire, won an Open Scholarship to read Medicine at Cambridge in 1979. He chose a Part II in Computer Science and after completing his medical degree at St Bart’s Hospital in London he trained in surgery in London, Cambridge and Wessex. At Southampton he was awarded his MS degree in 1994 for research on computer modelling the haemodynamics of occlusive arterial disease and was appointed a consultant vascular surgeon at Good Hope Hospital in 1999. Since then he has combined his experience in medicine, research and computer science to improve vascular surgery services at Good Hope. In 2004 his team were awarded the NHS Innovation Award for Service Delivery for the Leg Ulcer Telemedicine Service. His current projects include the application of discrete event simulation (DES) to the design of improved healthcare processes for which he was awarded the HITEA 2005 Best use of IT in the Health Service for the successful implementation of the DES-designed One Stop Vascular Surgery Clinic.